Best SOAP Notes with Examples & Free Template
For Social Workers, Case Managers, Therapists, Counselors, Clinicians, and other Healthcare Practitioners
Struggling to write a solid SOAP note? You’re not alone. Whether you’re a case manager, social worker, therapist, or any healthcare or medical professional, knowing how to structure your documentation properly can save time, improve communication, and help you deliver better care.
In this guide, we’ll show you exactly how to write effective SOAP notes assessments — with real-world examples, templates, and a free SOAP Note Writing Checklist – PDF & Word that you can start using today.
Let’s get started
Watch this overview video or read the detailed guide below.
What Is a SOAP Note?
A SOAP note is a simple yet powerful acronym that structures your client interactions, ensuring you capture all critical information to improve client care. SOAP stands for:
- Subjective: What the client or patient says
- Objective: What you observe or measure
- Assessment: Your professional interpretation
- Plan: What you’ll do next
The Soap note format helps professionals in health, mental health, and social services organize their thoughts, track client progress, and collaborate with others more efficiently.
- S – Subjective: This is the client’s story, in their own words. What are they telling you? Their chief complaint, feelings, concerns, symptoms, and relevant personal history.
- O – Objective: What did you observe or measure? This includes factual, unbiased data: vital signs, physical exam findings, lab results, your observations of their mood, behavior, appearance, or interactions during the session.
- A – Assessment: Your professional interpretation. Here, you synthesize the Subjective and Objective data. What are the client’s main problems or needs? What’s your working diagnosis or clinical impression? How is the client progressing?
- P – Plan: What are you going to do next? This outlines your strategy: interventions, referrals, follow-up actions, medications, and any education provided to the client.
Why Are SOAP Notes So Important?
Beyond just record-keeping, SOAP notes:
- Improve Client Care: They ensure continuity, so anyone reviewing the file can quickly understand the client’s journey.
- Boost Communication: Facilitate seamless information sharing among multidisciplinary teams.
- Provide Legal Protection: Serve as a clear, professional record of care provided.
- Support Billing & Reimbursement: Justify services rendered to insurance companies.
Pro Tip: Think of SOAP notes as storytelling with structure. The format ensures consistency without losing the unique details that matter.
SOAP Note Examples & Samples
“Soap note examples” are powerful learning tools. Let’s dig into how to populate each section with high-value information, touching on “mental health soap note example,” “therapy soap note example,” and the crucial “assessment part of soap note.”
Let’s get straight to what most professionals need — concrete SOAP Note examples. Whether you’re creating a general note as a social worker or need a specific therapy or medical SOAP note example, these SOAP samples can guide you.
| We’ll first cover SOAP notes for social workers followed by SOAP writing for therapists and other clinicians |
SOAP Notes for Social Workers: Tailoring Your Documentation
Social workers have unique documentation needs, and searches like “soap notes social work,” “social work soap note example,” and “soap case notes social work” show this clearly.
Your notes often involve complex systems, advocacy, and a broader ecological perspective. “Soap progress notes” are especially vital here for tracking client journeys through various interventions.
Actionable Steps for Social Work SOAP Writing:
- Holistic Subjective: In your Subjective section, include not just client feelings but also their reported experiences with systems, housing, employment, and social support.
- Document Systemic Interactions (Objective): If you made calls, attended meetings, or collaborated with other agencies on the client’s behalf, document these in the Objective section.
- Assess Environmental Factors: Your Assessment should go beyond individual pathology. Consider how social determinants of health, community resources (or lack thereof), and systemic barriers impact the client.
- Action-Oriented Plan: The Plan section is crucial for outlining advocacy efforts, resource linkages, coordination with other providers, and specific interventions to address social, emotional, and practical needs. “Soap method social work” emphasizes this comprehensive approach.
- Track Progress Broadly: Your “soap progress notes” should reflect not just individual change but also improvements in the client’s living situation, access to resources, and overall well-being within their environment.
Your Social Work SOAP Note Checklist:
- [ ] Subjective captures client’s feelings and their experience with social systems.
- [ ] Objective includes observations of client and documented actions related to systems/advocacy.
- [ ] Assessment considers the impact of social, economic, and environmental factors.
- [ ] Plan details concrete steps for resource connection, advocacy, and multi-agency collaboration.
- [ ] Progress notes clearly illustrate changes in the client’s life situation and well-being.
Social Work SOAP Recap
- Subjective: Client reports feeling “on edge” and unable to sleep for more than three hours per night.
- Objective: Client appeared anxious, fidgeting during the session. Elevated heart rate recorded.
- Assessment: Symptoms consistent with increased anxiety and insomnia.
- Plan: Begin weekly therapy sessions. Introduce basic relaxation techniques and monitor sleep patterns.
Pro Tip: Remember that “soap notes for social workers” often serve as a communication tool for a broad range of stakeholders – from court officials to housing authorities. Clarity, accuracy, and a focus on measurable outcomes are paramount.
SOAP Note Examples for Therapists, Counselors, Mental Health Specialists, and other Mental Healthcare Professionals
Imagine a therapy session:
- Subjective: “Client reports increased feelings of anxiety over the past week, stating, ‘I’ve been feeling overwhelmed and can’t seem to quiet my mind.’ Reports difficulty falling asleep, waking frequently, averaging 4-5 hours of sleep per night. Denies suicidal or homicidal ideation.”
- Objective: “Client arrived on time, appeared slightly fatigued but well-groomed. Maintained good eye contact. Speech was clear, coherent, and at a normal pace. Affect was congruent with reported mood (anxious). No overt signs of distress observed. Client actively participated in discussion.”
- Assessment: “Client presents with symptoms consistent with Generalized Anxiety Disorder, exacerbated by recent work stressors. Sleep disturbance is a significant contributing factor to current distress. Client demonstrates good insight into symptoms and is motivated for therapeutic intervention.”
- Plan: “1. Continue Cognitive Behavioral Therapy (CBT) techniques focusing on thought challenging and relaxation strategies. 2. Provide psychoeducation on sleep hygiene and stress reduction. 3. Explore potential benefits of mindfulness exercises. 4. Schedule follow-up appointment in one week to monitor progress and re-evaluate sleep patterns.”
Key Content for Each Section:
- Subjective (What They Say):
- Direct quotes (use quotation marks!).
- Client’s chief complaint and history of present illness.
- Relevant past medical/social history they report.
- Functional limitations reported by the client.
- Pro Tip: Capture the essence of their experience, not a transcript.
- Objective (What You See/Measure):
- Your observations: appearance, mood (your assessment, not theirs), behavior, affect, speech patterns.
- Relevant physical findings (e.g., vital signs, gait, posture).
- Results of standardized assessments (e.g., PHQ-9 score).
- Pro Tip: Be factual and non-judgmental. Stick to what’s observable.
- Assessment (Your Clinical Judgment – The ‘A’ in ‘Assessment part of soap note’):
- Diagnosis (if applicable): Clinical impression or diagnostic codes.
- Problem List: Identify the key issues from S & O.
- Progress: Note improvement, decline, or stagnation.
- Contributing Factors: Your professional opinion on what’s driving the issues.
- Strengths: Acknowledge client’s resources and resilience.
- Pro Tip: This is where you connect the dots between the subjective report and objective observations. Justify your thinking!
- Plan (What’s Next):
- Interventions: Specific actions you will take (e.g., “Provided psychoeducation on coping skills”).
- Client Homework/Assignments: Tasks for the client between sessions.
- Referrals: To other professionals or resources.
- Follow-Up: When the next session is scheduled.
- Goals: Short-term and long-term objectives (often linked to your Assessment).
- Pro Tip: Make your plan SMART (Specific, Measurable, Achievable, Relevant, Time-bound).
Recap:
- Subjective: Client discussed recent conflict with a partner, expressing guilt and frustration.
- Objective: Tearful during the session, avoided eye contact.
- Assessment: Interpersonal conflict contributing to depressive symptoms.
- Plan: Explore communication strategies in the next session. Assign journaling as homework.
Pro Tip: Save a few high-quality SOAP note examples in your notes folder or EHR system. They’ll serve as a model when you’re under pressure.
Building Blocks: Formatting & Templates That Work
One of the top questions is about “soap note format” and “soap notes template.” The good news? There’s a clear structure that makes writing them a breeze. Forget generic “soap notes template pdf” searches; we’ll show you how to truly leverage these tools.
Actionable Steps to Flawless Formatting:
- Strict Sectioning: Always clearly delineate each of the S, O, A, and P sections. Use bold headings or distinct paragraphs.
- Bullet Points for Clarity: Especially in the Objective and Plan sections, use bullet points to break up information and make it scannable.
- Consistency is King: Decide on a format you like and stick to it. This makes your notes predictable and easy to read for others (and your future self!).
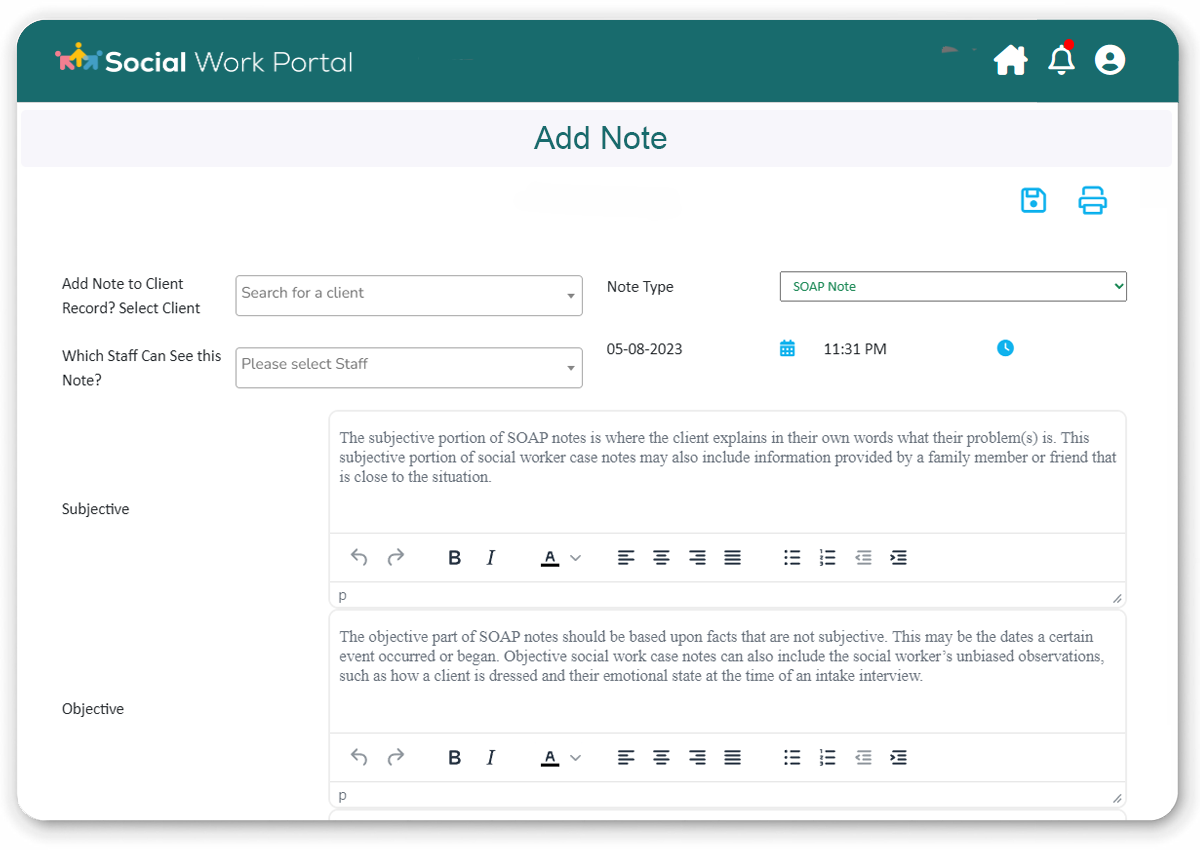
- Embrace Digital Templates: If you use an EHR, learn its SOAP note features. If not, create a master template in a word processor with pre-set headings. This saves immense time. Searching “online soap notes” tools can also reveal excellent integrated platforms.
Your Formatting & Template Checklist:
- [ ] Clear, distinct headings for Subjective, Objective, Assessment, Plan.
- [ ] Information in each section is relevant only to that section.
- [ ] Avoid lengthy prose; use concise sentences and bullet points.
- [ ] Consistent formatting across all your notes.
- [ ] Utilizing a digital template to streamline the process.
Pro Tip: Your “soap note template” isn’t a rigid cage; it’s a supportive framework. Customize it slightly for different client types or common interventions to make it even more efficient.
Using SOAP Notes in Mental Health and Counseling
SOAP notes are essential in mental health settings. They help track emotional changes, behaviors, medication effects, and risk levels.
Example: Mental Health SOAP Note
- Subjective: “I don’t feel safe at home,” client says, describing ongoing verbal abuse.
- Objective: Flat affect. Client avoided discussing specific events.
- Assessment: Indicators of emotional trauma. Client may be in an unsafe living situation.
- Plan: Provide resources for domestic violence support. Schedule emergency check-in within 24 hours.
Pro Tip: If you’re documenting high-risk situations like suicidal ideation or domestic abuse, always note referrals, safety plans, and immediate follow-up actions.
Writing SOAP Notes for Social Work
In social work, documentation often includes complex life situations, systems navigation, and community referrals. SOAP notes bring structure to this complexity.
Example: Social Work SOAP Note
- Subjective: Client shared missing three appointments due to lack of transportation and childcare.
- Objective: Case records confirm missed visits. No-shows noted on schedule.
- Assessment: Structural barriers are preventing client from accessing support services.
- Plan: Refer to transportation program. Connect with local daycare assistance program. Re-engage next week.
Social workers can also use SOAP note templates to document advocacy efforts, case updates, or client check-ins across multiple services.
Pro Tip: Social work SOAP notes should link directly to action steps — referrals, follow-ups, and updates to the client care plan.
Online SOAP Notes, PDFs, and Progress Tracking
Don’t want to start from scratch every time? Use tools and templates to streamline your documentation.
Here’s what professionals are using today:
- Online SOAP note tools that auto-fill common fields
- Downloadable SOAP note PDFs for quick handwritten use
- Pre-built templates that include assessment sections
- Digital systems to track SOAP progress notes over time
Pro Tip: Label your templates by service type (e.g., “Intake,” “Check-in,” “Crisis Session”) to make documentation faster and more consistent.
Quick SOAP Note Writing Checklist
Use this checklist to make sure your note is clear, complete, and ready to go:
✅ Subjective – Did I capture what the client or patient said in their own words?
✅ Objective – Did I document observable facts like behavior or test results?
✅ Assessment – Have I clearly explained my interpretation or diagnosis?
✅ Plan – Did I outline next steps, timelines, or referrals?
✅ Tone – Is it professional, respectful, and neutral?
✅ Spelling & Grammar – Did I proofread before saving or sending?
✅ Format – Does it follow the proper SOAP note structure?
✅ Storage – Is the note saved securely in the right location?
👉Download the Full Soap Notes Checklist – PDF & Word
Get Additional Free SOAP Templates below
Are you looking to use the SOAP subjective objective assessment plan format for your client or patient progress notes? We have two printable SOAP notes downloads that you can leverage to enable your work.
The first is a therapy SOAP note example PDF that you can download, print out, and reference to help you better understand SOAP notes meaning when writing your own.
The second is a blank SOAP assessment template for you to use. It includes the four sections of the SOAP format example: Subjective, Objective, Assessment, and Plan.
Sign Up to Download a SOAP Note Example PDF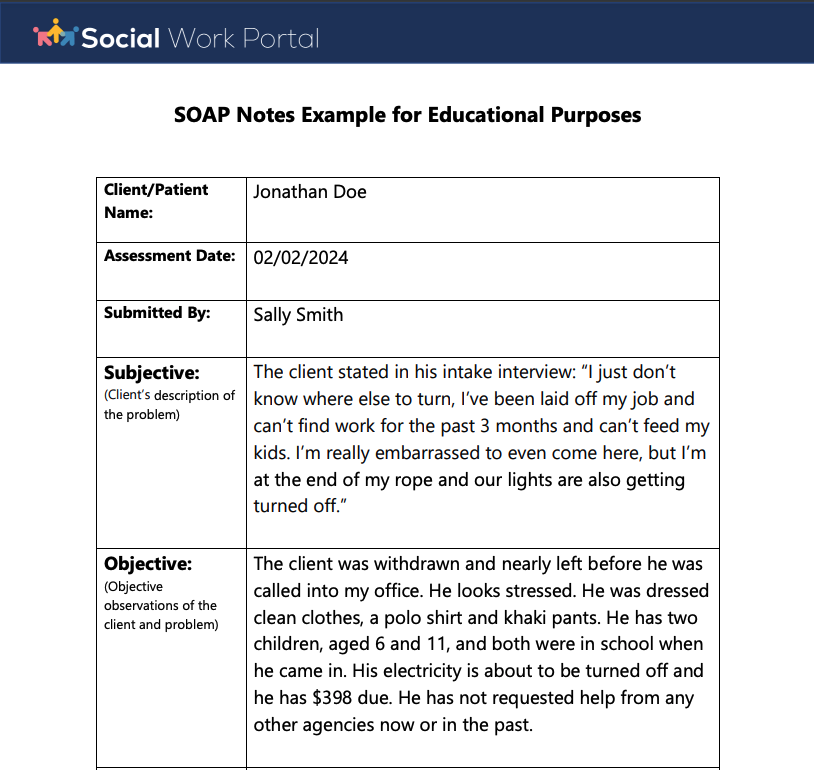
Sign Up to Download a Blank SOAP Format Example Template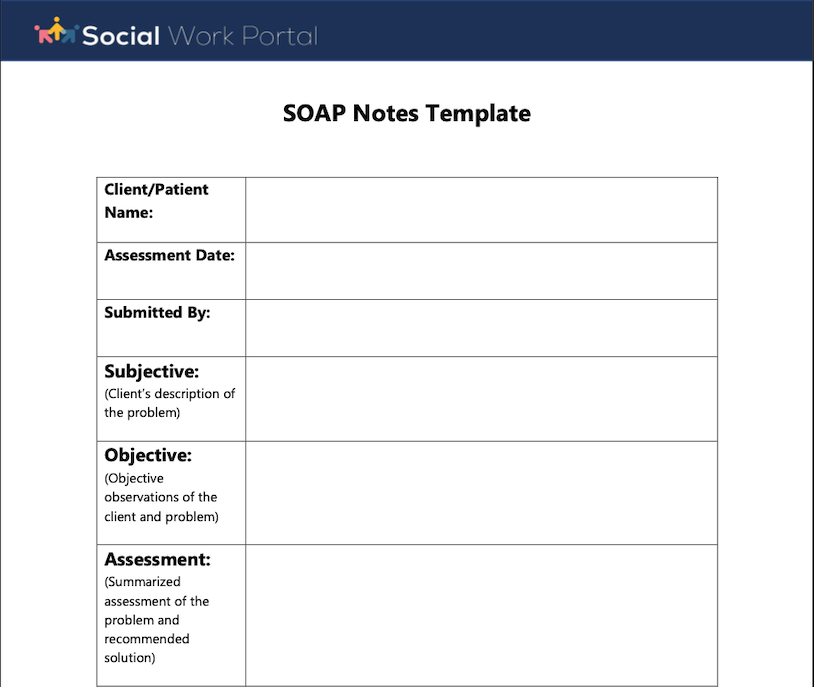
Once you sign up for a free trial, visit ‘My Free Tools’ in the menu to download these and other freebies!
Don’t Miss: Assessing Risk in Social Work – Everything You Need to Know
Pro Tip: A well-written SOAP note tells a story: where your client is now, what’s changing, and where they’re headed next.
Final Thoughts
SOAP notes don’t have to be overwhelming. With the right examples, templates, and structure, you can write powerful notes that support your clients and make your work easier.
Whether you’re in mental health, counseling, or social work, the ability to quickly produce accurate, professional SOAP notes is one of the most valuable skills you can develop.
By consciously applying these strategies, you’ll transform your note-taking from a burden into a powerful asset. You’ll save time, improve communication, and most importantly, enhance the quality of care you provide. Start small, be consistent, and watch your SOAP note skills—and your practice—flourish!
Want to Make Documentation Even Easier?
Explore our other free tools and templates, including downloadable SOAP note examples, PDF formats, and full case management systems designed for social workers and health professionals.
📝 Start documenting smarter today.
Note: Content on this website (socialworkportal.com) is copyrighted and protected under applicable copyright laws. Unauthorized reproduction, distribution, or use of any content from the website, without explicit written permission, is strictly prohibited. Read: Terms of Use.
Social Work Portal Disclaimer: Social Work Portal is not a social work agency and we do not refer social workers. This web site is provided for educational and informational purposes only and does not constitute providing medical advice or professional social and healthcare services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with ... Read our full disclaimer here: Social Work Portal Disclaimer.
Want to Read More. See below for our previous article
SOAP Notes Explained – Everything You Need to Know about SOAP Notes
Best Guide on What You Need to Know: SOAP Note Examples, Meaning, Tips & More
When a therapist, mental health care provider, nurse, or other health care professional meets with a patient, the session is typically documented. These notes become a very important part of the patient’s health record.
What happened during the session? How is the individual progressing in their treatment? What is the professional’s assessment and plan for their continued care? This is some of the information that is documented in these meeting/session notes.
How those notes are formatted is where SOAP notes come in. The SOAP documentation method is one of the most popular ways to format these session notes. SOAP clinical notes are used throughout the medical and mental health professions and social work community.
Assessment in SOAP Note
Writing SOAP Notes keeps documentation consistent and has other benefits, such as providing a streamlined way to write down important information about each patient meeting.
Learning SOAP note taking can make the job of documenting progress notes and client interactions easier. Using the four parts of a SOAP note can also improve the accuracy and completeness of these notes.
In this Social Work Portal article, we’ll review the importance of SOAP notes and go through SOAP method case notes in detail. We’ll also go through several SOAP format examples.
Also…don’t miss our free SOAP case notes example and template that you can download from our All-in-One Client & Case Management Software.
See Also: Social Work Case Notes Formats (SOAP, BIRP, GIRP, and DAP Notes Examples)
Table of Contents: SOAP Notes Social Work
Keep on scrolling down this page to read each section or click any link below to go directly to that section.
- SOAP Notes Meaning
- What Is the Benefit of Using the SOAP Note Format?
- S in SOAP Note Form (Subjective)
- O in Soap Note Acronym (Objective)
- A in Soap Note Structure (Assessment)
- P in Soap Format (Plan)
- Tips for Writing Good SOAP Therapy Notes
- SOAP Notes Examples for Social Workers
- Downloads: SOAP Note Assessment Example & Free SOAP Format Word Template
- Conclusion | SOAP Note Format & How to Write a SOAP Assessment
- FAQ | SOAP Case Notes
Don’t Miss: What You Need to Know About the HIPAA Form for Patients to Release Medical Information
SOAP Notes Meaning
SOAP in medical terms was introduced by Lawrence Weed, MD, almost half a century ago. The SOAP form of taking notes came from the problem-oriented medical record (POMR).
The SOAP note documentation style was designed to distill complex and detailed information into an organized format that focuses on four key areas, which we’ll explain below.
How do you define SOAP notes?
SOAP notes are a framework for documenting information related to a patient interaction, such as a meeting or session. A SOAP note is typically part of a patient’s chart or record.
SOAP acronym
Here is what each of the letters in SOAP note stands for:
- Subjective
- Objective
- Assessment
- Plan
These four terms in a SOAP note plan example represent different note sections. You can think of the parts of a SOAP note as headers. The social worker or therapist uses these headers to organize the session notes in a consistent manner.
Shortly, we’ll go through each area of SOAP case notes social work professionals and medical practitioners use and explain the types of details entered into each SOAP acronym.
Related: What You Should Know About a Medical Records Release Authorization Form
Do you have any questions or feedback about this article on therapy SOAP note example, SOAP notes physiotherapy, and an assessment in SOAP? If so, click here to contact the Social Work Portal Team.
What Is the Benefit of Using the SOAP Note Format?
Why is the subjective objective assessment plan format in SOAP notes so popular? Besides being around for nearly 50 years, the SOAP note example is a simple, yet effective method for organizing patient progress notes.
Here are some of the benefits of adopting a SOAP note plan for your patient documentation:
- Improves note-taking efficiency
- Helps providers formulate treatment strategies
- Ensures completeness of progress notes
- Widely used in the social work & medical communities
- Helps providers communicate information with team members
- Organizes patient session documentation
- Reduces miscommunication between healthcare professionals
Are you ready to increase your capacity with a platform that includes case notes, intake, and assessment templates? Sign up for a free trial of our social work client management application.
In the next sections, we will dive into each of the four sections of the SOAP model case notes format, beginning with the “s” for subjective in SOAP note format case notes.
Popular Article: Social Work Theory & Practices You Need to Know About
Are you looking for free social worker templates & forms? You can sign up to download all our free social worker tools here.
S in SOAP Note Form (Subjective)
The first letter in the SOAP subjective objective assessment plan framework is “S” for subjective. Subjective in SOAP note methodology is the area of your notes where you include the patient’s subjective description of their situation.
This could be how they are feeling, or what they think of their environment, progress, or situation. You might want to start a subjective SOAP note example with “The client feels…” or “The client stated…”
The SOAP note guide for this subjective area is to include the patient’s perspective. You may also include the perspective of the patient’s family if you met with them during the session.
Read More: In-Person & Online Social Work Programs
Do you have a de-identified SOAP progress note example or mental health SOAP note example that you feel would be helpful to share with other social workers? If so, click here to contact the Social Work Portal Team.
O in Soap Note Acronym (Objective)
The next acronym in the SOAP writing method stands for objective. This section is for the social worker, medical, or mental health professional to enter their objective observations of the patient and the patient’s situation.
The objective in SOAP note format should contain measurable and observable details. Think of this section as one to enter facts and data, not opinions or feelings.
A SOAP note objective example would be the number of times a patient took drugs since the last session, or it might be another preset measure of progress toward therapy goals.
Another SOAP objective example would be observations about the patient. Such as, “The individual had a large bruise on their left cheek that was not there at our last session two weeks ago.”
Related: Different Social Workers You May See & What They Do
A in Soap Note Structure (Assessment)
The assessment section of SOAP note templates is the appropriate place for the mental health or medical professional to add their opinions about the client’s situation and assessment of progress during this session or meeting.
Assessment in SOAP note forms is where you will sum up what is going on in the “S” and “O” portions of the SOAP form and give your professional opinion of what that means.
A SOAP assessment example might be that the client is progressing well in dealing with self-doubt issues, but still needs to work on their anxiety issue, which seems to be getting worse.
The SOAP format social work, medical, or mental health assessment includes the professional’s clinical interpretation of the client’s current situation and/or progress in their treatment plan.
Don’t Miss: Clinical, Medical & Hospital Social Worker Guide – All You Need to Know
P in Soap Format (Plan)
The final section of the progress note SOAP format is for plan. This section is where you will write down your next steps in the patient’s treatment plan.
When using SOAP format case notes, the plan area should be tied into your ongoing treatment plan for the individual and may refer to past session SOAP notes.
Based on your assessment of the client’s progress, include any short-term or long-term plans that you are implementing or recommending. For example, your social work case notes SOAP plan section might state that the individual is being sent to a drug rehabilitation facility. Or it could note a reduction in sessions because the patient is progressing well in therapy.
The plan will be what your next session’s SOAP follow up note will reference when assessing progress toward goals.
Do you have any questions about the difference between soap objective example and soap note plan example? Or do you have feedback about the best mental health soap note example that has worked well for you? If so click here to contact the Social Work Portal Team.
Tips for Writing Good SOAP Therapy Notes
As you can imagine, during a patient or client session a lot of different information will be collected. This includes how the patient is feeling or dealing with the issue being addressed, what the health care professional is observing about the situation, their assessment, and what to do next.
The SOAP note format example provides a way to take all that information and create organized and meaningful case and progress notes. To get the most out of SOAP progress notes, we have some tips you can use.
 |
More Capacity. More Time.
x Simple Software for Social Workers |
Good Soap Note Example Tips:
- Keep notes to 1-2 pages and focus on the most important information that needs to be documented.
- Keep the content unique to this session, don’t just repeat the prior session notes.
- Avoid personal judgments and the use of “good” or “bad” to describe behavior.
- Make statements that are supported by measurable or observable information.
- Notes should be easy to read. Type online SOAP notes into a form or app, or if writing SOAP notes by hand, make sure they are legible.
- Don’t use unsourced opinions.
- Describe ongoing plan progress and next steps, rather than recreating your plan in every SOAP assessment example.
Popular Article: Social Work Interventions for Social Workers | All You Need to Know
SOAP Notes Examples for Social Workers
To help you better understand SOAP note guidelines, we’ve included three SOAP note example scenarios below. These are fictitious and designed for educational purposes.
You’ll also note that the SOAP note assessment examples below are short to provide brief examples for you to get the general idea of the SOAP framework. Your SOAP progress notes will likely be a bit longer.
Pediatric SOAP Note Example
|
Social Worker Software – SOAP Notes Template – Built-in Assessments Sign up today and improve the way you work! |
|
SOAP Notes Counseling Example
Psychiatric SOAP Note Example
| Subjective: | Elaine is still feeling very depressed and isolated. She states that she occasionally “hears voices, but I can’t make out what they are telling me.” She doesn’t like the side effects of her prescribed medication but admits that it helps her symptoms. |
| Objective: | Elaine’s clothing looks unwashed, and her appearance is disheveled. She speaks in a rushed fashion. |
| Assessment: | The lack of progress is concerning. Elaine has auditory hallucinations, a key indicator of schizophrenia. |
| Plan: | Elaine’s medication is being changed to Aristada Initio at 675 mg. The next session with Elaine is in three days. |
See Also: How Do Social Workers Really Do Eco Mapping In Social Work?
Do you have questions about any SOAP note example that we’ve provided, like the SOAP notes counseling example? Do you need more references about SOAP in medical terms? If so, click here to contact the Social Work Portal Team.
Downloads: SOAP Note Assessment Example & Free SOAP Format Word Template
Are you looking to use the SOAP subjective objective assessment plan format for your client or patient progress notes? We have two printable SOAP notes downloads that you can leverage to enable your work.
The first is a therapy SOAP note example PDF that you can download, print out, and reference to help you better understand SOAP notes meaning when writing your own.
The second is a blank SOAP assessment template for you to use. It includes the four sections of the SOAP format example: Subjective, Objective, Assessment, and Plan.
Sign Up to Download a SOAP Note Example PDF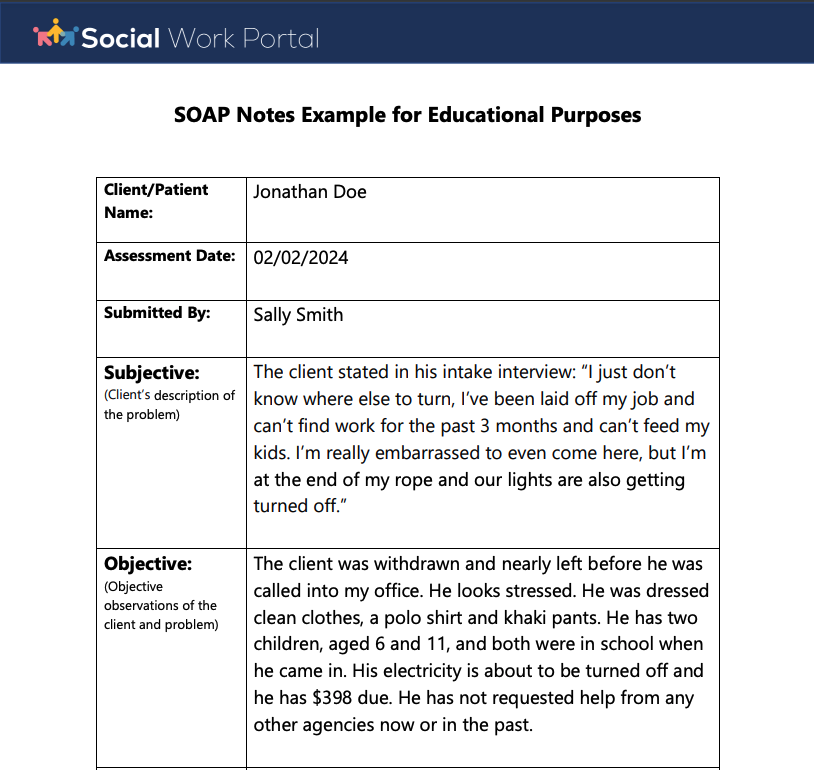
Sign Up to Download a Blank SOAP Format Example Template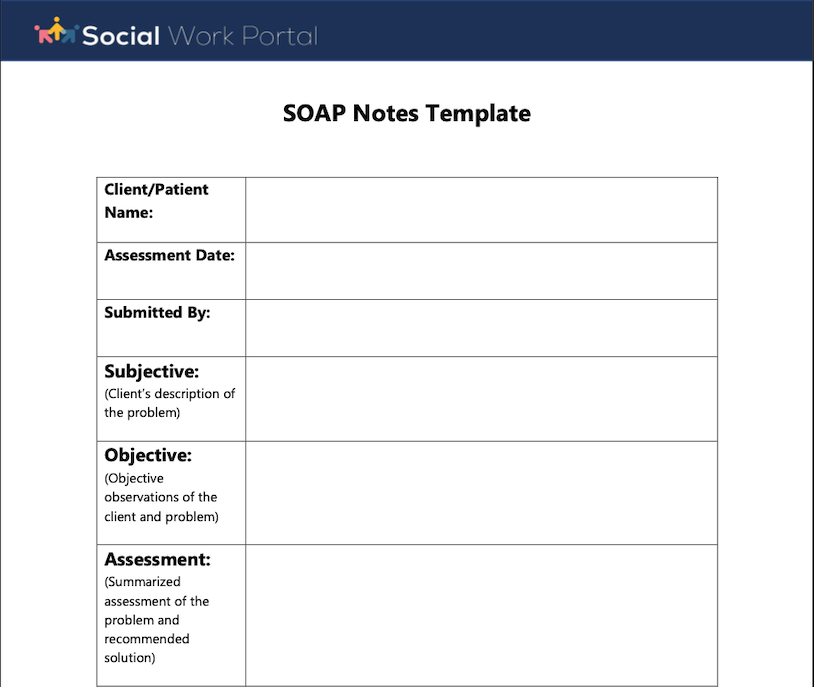
Once you sign up for a free trial, visit ‘My Free Tools’ in the menu to download these and other freebies!
Don’t Miss: Assessing Risk in Social Work – Everything You Need to Know
Do you have any feedback about this article or need additional soap note objective examples? If so, click here to contact the Social Work Portal Team.
Conclusion | SOAP Note Format & How to Write a SOAP Assessment
The SOAP acronym and SOAP note assessment example has proven to be an efficient way of documenting patient and client case notes. It provides a repeatable and consistent method of relaying complex information.
Anyone in the social work or medical field should study at least one SOAP format example to familiarize themselves with this popular note-taking framework.
Whether you use SOAP notes physiotherapy templates, social work SOAP notes, or SOAP in medical terms, this flexible format should be a key tool in your patient documentation toolbox.
For questions about the main objective in soap note taking or feedback on the best soap documentation method, click here to contact the Social Work Portal Team.
Is there something else you’d like to know about soap clinical notes, soap model case notes, or soap note guidelines? If so click here to contact the Social Work Portal Team.
FAQ | SOAP Case Notes
What are the 4 parts of SOAP?
SOAP note stands for four key sections for organizing patient or client session notes. The four parts of SOAP are Subjective, Objective, Assessment, Plan.
How do you make SOAP notes?
Writing SOAP notes means following the SOAP format, beginning with the S in SOAP note, which stands for Subjective. In this area, the subjective feelings and opinions of the patient are noted.
Next is the O in SOAP notes, which is for Objective. This is where the health care professional will include their objective observations of the patient.
The A in SOAP note is for Assessment. This is the section where the health care professional will describe their assessment of the patient and their situation.
The P in SOAP stands for Plan. The next steps for the patient to take are included in this part of a SOAP note.
What is the benefit of using SOAP notes?
Here are some of the benefits of adopting a SOAP note plan for your patient documentation:
•Improves note-taking efficiency
•Helps providers formulate treatment strategies
•Ensures completeness of progress notes
•Widely used in the social work & medical communities
•Helps providers communicate information with team members
•Organizes patient session documentation
•Reduces miscommunication between healthcare professionals
How do you take good SOAP notes?
Good Soap Note Tips:
•Keep notes to 1-2 pages and focus on the most important information.
•Keep the content unique to this session.
•Avoid personal judgments and the use of “good” or “bad.”
•Make statements that are supported by measurable or observable information.
•Notes should be easy to read.
•Reference your ongoing plan progress and add to it.
Note: Content on this website (socialworkportal.com) is copyrighted and protected under applicable copyright laws. Unauthorized reproduction, distribution, or use of any content from the website, without explicit written permission, is strictly prohibited. Read: Terms of Use.
Social Work Portal Disclaimer: Social Work Portal is not a social work agency and we do not refer social workers. This web site is provided for educational and informational purposes only and does not constitute providing medical advice or professional social and healthcare services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with ... Read our full disclaimer here: Social Work Portal Disclaimer.
Image sources: Stock.adobe.com